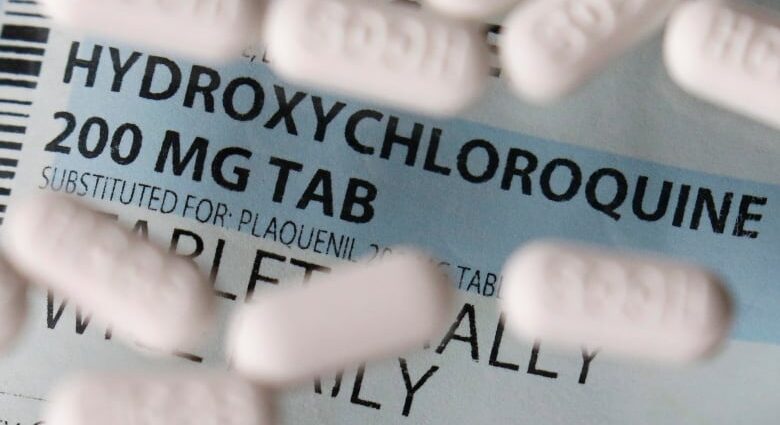
The drug hydroxychloroquine, which has been the subject of heated debate as a potential treatment for COVID-19, was not effective in preventing the disease in Canadians and Americans at high risk, according to the first gold standard clinical trial.
In Wednesday’s issue of the New England Journal of Medicine, medical researchers reported on testing the use of hydroxychloroquine in 821 adults in the U.S. and in Quebec, Manitoba and Alberta. The participants did not have symptoms but were exposed to someone with confirmed COVI9-19 in a health-care or household setting.
Hydroxychloroquine is often used to treat autoimmune diseases such as lupus. U.S. President Donald Trump said he’s taken hydroxychloroquine, although he’s not tested positive for the coronavirus infection. No studies have proven this drug or any others are effective against COVID-19.
The exposures were all considered high risk because the participants were less than two metres away from a confirmed case for more than 10 minutes without wearing a mask or face shield. The goal of the randomized trial was to see if hydroxychloroquine could prevent symptoms of infection, known as post-exposure prophylaxis, compared with taking a sugar pill.
“In this trial, high doses of hydroxychloroquine did not prevent illness compatible with COVID-19 when initiated within four days after a high-risk or moderate-risk exposure,” the study’s authors wrote.
Gold standard method
Dr. Emily McDonald, a physician at the Research Institute of the McGill University Health Centre, co-authored the randomized control trial in which half of participants were randomly assigned to the drug and half to the placebo without investigators knowing to avoid bias in interpreting any symptoms or their resolution.
McDonald called it the gold standard method to have the best evidence to support how to prevent spread of COVID-19.
“When we politicize the drug and we stop studies early for reasons that are perhaps not entirely valid, we risk never answering the question properly because the enrolment for the studies drops off,” McDonald said.

Overall, 107 of 821 of participants developed COVID-19 based on a swab or compatible symptoms during 14 days of followup.
No deaths occurred
Of those who received hydroxychloroquine, investigators said 49 developed the disease compared with 58 in the placebo group, a difference that could simply be random.
Two patients were hospitalized, one in each group. No deaths occurred.
Medication side-effects such as nausea and abdominal discomfort were more common for patients taking hydroxychloroquine compared to placebo (40 per cent versus 17 per cent), but no serious treatment-related adverse reactions were reported, including any heart arrhythmia.
Earlier on Wednesday, the World Health Organization announced it was resuming the hydroxychloroquine arm of its global Solidarity trial into potential treatments for COVID-19 following a pause to check for any potential safety concerns such as heart problems.
“WHO’s very much in favour of and encourages the continuation of randomized trials that are looking at different drugs to reduce mortality but also to reduce the severity of the illness,” Dr. Soumya Swaminathan, WHO chief scientist, told reporters.
Other results expected soon
The Solidarity trial includes participants and researchers in Canada.
Dr. David Boulware, the trial’s lead researcher and an infectious disease physician at the University of Minnesota, said results of another placebo-controlled trial are expected soon, this one testing hydroxychloroquine as a coronavirus treatment, rather than to prevent infection.
Whether the drug can be given as an effective treatment sooner either in the community or in the hospital remains to be answered, McDonald said. But so far, results suggest it’s safe to continue studying it.
Participants for the trial were recruited online. They ranged in age from 33 to 50, and most were health-care workers. They did not have underlying health conditions that could make taking the drug dangerous.
Dr. Michael Hill is studying hydroxychloroquine as a treatment for COVID-19 at the University of Calgary as part of another clinical trial that was paused. Hill was not involved in the newly published study and said it’s not surprising if the public is confused about the drug given the promotional messages from political leaders like Trump and Brazil’s president Jair Bolsonaro.
“I’m sure when we look back at it, we’ll use it as a case history example,” Hill said. “But I hope we get stronger and stronger oversight of the science irrespective of what happens next.”
Previous studies of hydroxychloroquine were observational in design, which greatly increases the potential for bias when managing patients, compared with a well-conducted, randomized clinical trial.
With files from CBC’s Vik Adhopia and Reuters